A Heart-to-Heart on Skin-to-Skin
How kangaroo care helped me survive my baby’s hospitalization
For parents, the physical separation from their baby can be one of the most distressing aspects of a NICU stay. Image credit: Watercolor by Veronica Tremblay for The Science Writer
by Jacqueline Sears
November 9, 2024
When my daughter Winslet was born 15 weeks early — weighing just 2 pounds, her translucent skin like a jelly coat, her eyes still fused shut — I wasn’t ready to be without her just because my body had let her go. Connected to a ventilator, umbilical catheter, and monitors, she incubated six floors above me in the neonatal intensive care unit (NICU). When I was discharged from the hospital less than two days later, the river near my house was rushing angrily, the winter trees were naked in their vulnerability, and my sorrow absorbed the gray landscape. I knew from experience how much it would hurt to be away from her.
On an ordinary Thursday afternoon five years earlier, 33 weeks pregnant with my second child, my water broke and began to trickle out. My son Merritt was born the following day. Doctors called it preterm premature rupture of membranes. I was blindsided. My first NICU experience was a microcosm of detachment. For years, I grieved what we had lost because of his early birth and the month-long hospitalization that followed. The trauma was etched into my mothering story, and I couldn’t imagine reliving it. With time, my desire for another baby compelled me to risk the possibility of another NICU stay. I would brave the dread that my baby could be born early — or worse. I wanted to believe it had all been an unlucky strike, and I was determined to reclaim my power.
When I discovered I was pregnant again on the night of a rare supermoon in September 2015, the sky was tinged pink. I took it as a sign and embraced our joy without pause for what the future could hold. Though my heart was all-in those first few weeks, I was soon in survival mode, suffering a long bout of morning sickness and a rollercoaster of intermittent bleeding. At 11 weeks, we learned we were having a girl. After two boys, I was buoyed by a brief swell of energy. At 17 weeks, clinging to my perinatologist’s optimism for a term pregnancy, we named our daughter, and I bought a tiny felt banner to hang over her nook in our bedroom. I began to feel at ease and allowed myself to imagine carrying her into the summer months; she would be born healthy and on time. At 19 weeks, my hope was punctured when a follow-up appointment revealed my cervix was funneling, an indication of early cervical dilation and — I would later learn — the cause of my successively shorter pregnancies.
We continued in a swift downward spiral with an emergency cervical stitch, then bed rest, and eventually, a hospital admission that took me away from my family until she was born. In March, after two episodes of preterm labor and a transfer to Virginia Commonwealth University Medical Center, contractions began again. The string that had given Winslet a chance to live at all was removed, and there was no turning back. I surrendered to a second birth where our story’s timing was all wrong.
Winslet had dedicated nurses who, like physiological magicians, orchestrated her bodily systems around the clock for the first three weeks of her life. I wondered if she would survive. If she did, would she be whole? The omnipresent tension of life and death was harrowing. Yet it was the pain, fueled by our early separation, that was the most disorienting and relentless. Holding her was the only salve to my anguish.
***
Parents of NICU babies are at higher risk than other new parents for developing perinatal mood and anxiety disorders (PMADS), including anxiety and depression. The loss of their caregiving role and physical separation from their newborn are among the most distressing factors they’re made to endure.
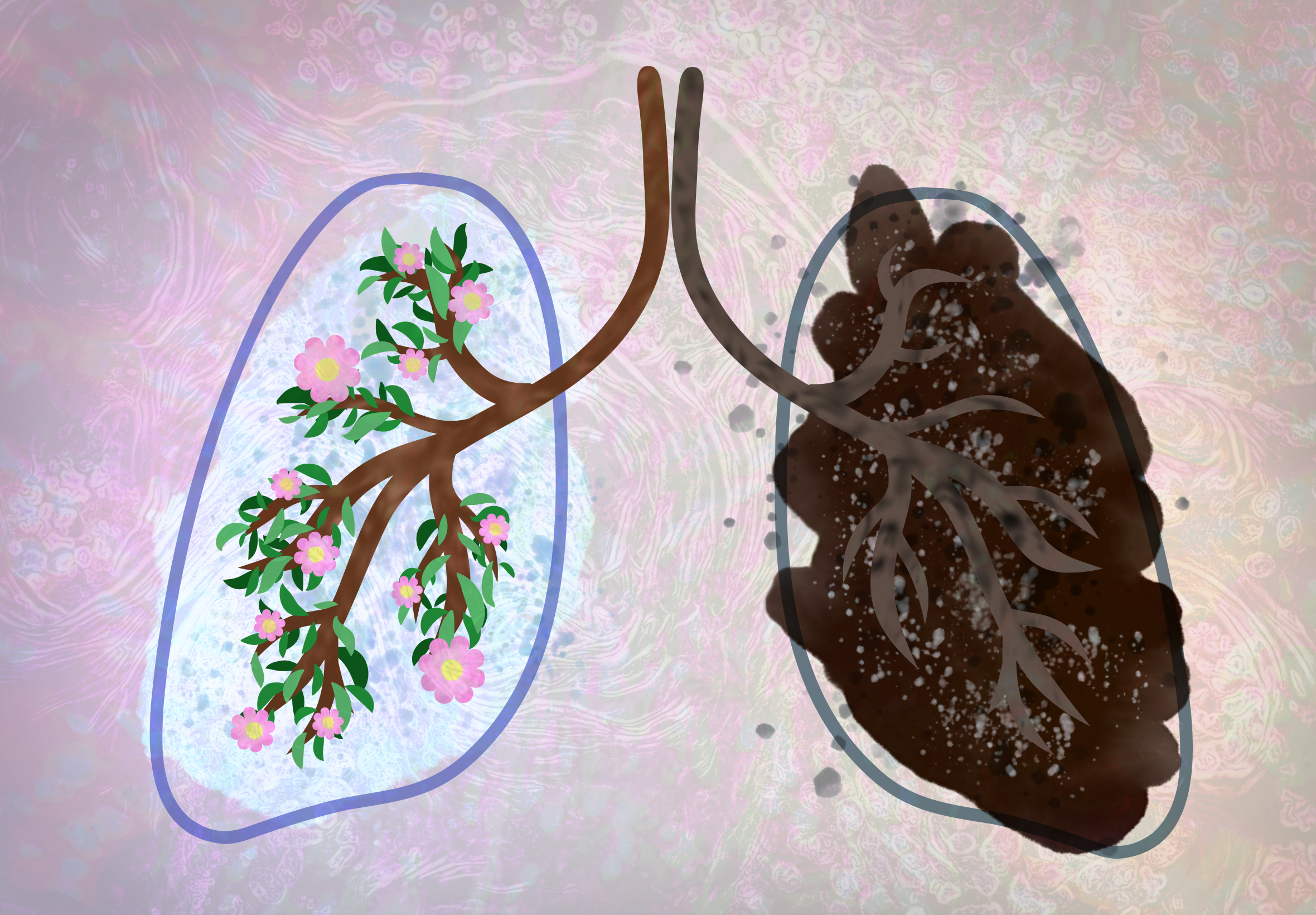
Parents who practice skin-to-skin care with their newborns may feel less stress and anxiety, and be less likely to experience severe postpartum depression. Image credit: Watercolor and ink by Veronica Tremblay for The Science Writer
Skin-to-skin care (SSC) is a nursing-supported parenting intervention that helps reconnect babies and parents. It is as simple as a parent holding their baby, skin to skin, on their chest.
While the benefits of SSC for babies are often celebrated, those for parents are less promoted — especially the potential of SSC to protect parents’ mental health. Recent data show that SSC reduces stress, anxiety, and depression for mothers with preterm and low-birth-weight infants. A 2023 systematic review of the effects of SSC reported that mothers who held their babies were 24% less likely to experience moderate to severe symptoms of postpartum depression.
Preterm birth has never been an easy path for new parents. In the 1800s, babies born early were certain to die. Medicine referred to premature babies as weaklings, and society pathologized their underdeveloped features in folklore and justified infanticide for these children whose fate seemed predetermined. The science of neonatal medicine emerged around the turn of the century, following the invention of a primitive version of the modern incubator in the 1890s. The first hospital unit for premature babies was established in Chicago in 1922. A parent’s primal desire to touch and hold their newborn has not always been recognized or valued. It was standard practice to separate babies and parents for the first 50 years of NICU care.
In the 1970s, Edgar Rey Sanabria, M.D., and Hector Martinez-Gomez, M.D., neonatologists and researchers in Bogota, Columbia, were working in a hospital with more babies than incubators, where infection and a lack of resources meant 70% of premature newborns died. Their chance observation in a remote village of a wet nurse with a small baby wrapped to her chest skin to skin, and her accounts of success caring for babies in this way, inspired them to consider its application in the hospital setting. They made a connection with kangaroos and other marsupials that carry their undeveloped young in protected pouches, where they latch onto a nipple, stay warm, and grow. Sanabria came up with the idea of mothers as incubators, calling it kangaroo care, and began placing babies on their parents’ chests. Survival rates went up, and infection rates went down. Now called SSC, the practice was effective at regulating body temperature and other stability markers like heart rate, respiratory rate, oxygen level, and sleep patterns. SSC is an intervention now implemented in more than 50 countries, including the United States. It is recognized as an opportunity to improve neonatal pain management and help build a healthy microbiome as well as offer social and psychological benefits for parents.
***
The first time I held Winslet, she was 36 hours old, intubated, and struggling for her life. A team of synchronized hands juggled cables and equipment as one of her nurses, Leslie Armstrong, transferred my baby in two cupped palms from the incubator to my chest. I remember our shared heat, her gummy fingers finding traction on my skin, and the joy of feeling her spontaneous kicks and stretches as I had just days earlier when pregnant. It was the first of hundreds of hours we would share, skin to skin, over the following 3 ½ months.
Armstrong took care of me too. She kept me oriented and steady in the unfamiliar, unforgiving, and often terrifying NICU world. She listened and helped me realize my attachment and breastfeeding goals. I was curious how she had the confidence in the beginning to support me in holding my tiny, sick baby. “It just takes a little creativity,” she told me over the phone eight years later, her warm voice a familiar comfort. “I knew how important it was to you. You needed it — maybe more than she did.”
Armstrong, who has dedicated her nursing career to neonatal intensive care, is also a mother who experienced the loss of her 3-year-old son to cancer shortly before we met. “When you suffer a loss like that, you’re not really afraid to do anything else for somebody, because you don’t want them not to have that opportunity,” she said. “If it’s important to them, then it needs to happen — no matter what, whatever we need to do.” Armstrong trusted Winslet and me, and she prioritized our relationship, knowing that every day in the NICU is a gift. Not every family gets to take their baby home.
“Everybody handles situations differently, and everybody needs different things,” Armstrong said. “That’s just part of being a nurse sometimes — it’s knowing what people need and really advocating for it to happen.” After being in a similarly powerless place, she tries to meet people where they are. “To know what it’s like to just be completely out of control and not be able to do anything for your kid, I think that drives my practice a lot too.” She believes it takes courage for parents to hold their baby and not fixate on the beeps and alarms. “Let us pay attention to the monitor, and let us work with the respiratory therapy team. You enjoy your baby, and we’ll take care of the rest.”
Armstrong had partnered with me to have SSC under conditions that were pushing the envelope at the time, given Winslet’s health status and the high level of respiratory support she required. This opportunity was not only the result of Armstrong’s advocacy on behalf of parents and babies but also a culture shift that had just begun within the medical community.
In 2015, the World Health Organization (WHO) published recommendations to improve preterm birth outcomes. These included a strong recommendation for Kangaroo Mother Care (KMC), which WHO defined as skin-to-skin contact as soon after birth and for as long as possible, paired with exclusive human milk feeding.
The following year, in response to the WHO’s guidance and after a thorough review and analysis of the evidence in middle and high-income countries, an international policy statement was endorsed and signed by health organizations, including the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, and the American College of Nurse-Midwives. It recognized their commitment to advocate for and implement KMC to “promote and accelerate” its use as the “standard of care for all small babies.”
In 2022, after conducting a study that had been halted because the KMC intervention showed such promise that it was unethical to withhold it from the control group, the WHO went a step further to recommend immediate Kangaroo Mother Care (iKMC) — placing baby on mom’s chest immediately after birth, instead of waiting for conventional stability criteria to be met — as a routine standard of care for all preterm and low-birth-weight babies.
The American Academy of Pediatrics in 2023 published a series of educational resources to promote iKMC and support a “paradigm shift to zero separation between mothers and their newborn babies with a goal to improve quality of care and outcomes for small and sick newborns.”
At Armstrong’s institution, she says, the emphasis on SSC has grown in the last eight years. The practice of SSC as a NICU care standard was still new when Winslet was born, especially considering it can take years to translate evidence-based guidance into policy. Now, prioritizing kangaroo care for every baby and family is the norm, Armstrong says. “I’m very pro-kangaroo care. All babies should be held every day,” she said. “If a mom has two hours at the NICU, let’s get holding.” She stresses the importance of communication between parents and the nursing team. “If a parent senses their nurse isn’t comfortable — and you can tell by looking at their face when you ask to kangaroo,” she laughed, “then ask them to talk to the nurse manager to help them. They just need more practice. I tell novice nurses, too, ‘If it makes you nervous, call me or the charge nurse — you don’t ever have to do it alone.’ The more they do it, the more comfortable they will become.”
While SSC is increasingly accessible, parental advocacy is still paramount. Racial and ethnic disparities exist in NICU care delivery. A 2021 study in the Journal of Developmental and Behavioral Pediatrics found differences in the rate, frequency, and duration of SSC for parents with low socioeconomic status and for parents who spoke a language other than English. Parents do better when they know what they want, feel confident and empowered to communicate their needs, and ask directly for SSC. Parents need to know they can request a medical interpreter and have the right to receive those services.
As interest in and awareness of postpartum mental illness has increased, family-centered NICUs have seized the opportunity to tackle the issue. Though policies and practices remain inequitable, more attention is being paid to how holding newborns skin-to-skin is essential for parents’ well-being. NICU parents are 20% to 40% more likely than parents with healthy newborns to experience anxiety, depression, and traumatic stress — one study reports as high as 70% of parents experience postpartum depression during or after a NICU stay. The earlier and smaller a baby is born, the more likely parents will be impacted. And NICU parents remain at higher risk for PMADS after hospital discharge and into the first year as they adjust to managing their baby’s ongoing health needs and transition to parenting independently at home.
***
Winslet’s early birth, medical fragility, and the marathon of being without her crushed me. I hung in a dark limbo those first days when her immature lungs, like tiny bricks, didn’t respond to treatment. It took weeks before she got the hang of life outside. Watching her through isolette walls, bearing witness to her pain during needle sticks and procedures, worried waiting for brain-bleed scans and blood transfusion after blood transfusion. Parts of me were numb. In her absence, I pumped breastmilk around the clock every few hours to establish a milk supply. During the day, I cared for my boys, who were 5 and 6, counting down the hours until my husband would return from work and it was time to traverse the highway between our home and the hospital, back and forth, traveling between my two worlds. As Winslet grew, I spent more time in the NICU and less time at home, but in the beginning, the evening hours were for us. At my leaving I would tuck her in, the goodbye always long. For most of her NICU stay, I was afraid to love her too hard, and also afraid I wasn’t loving her enough. To be separated from my vulnerable newborn was an unnatural reality that my body was unwilling to accept.
***
Kangaroo care is beneficial for both newborn babies and their parents. Image credit: Watercolor and ink by Veronica Tremblay for The Science Writer
When a parenting journey is stressed by such disruption in bonding and attachment, the sympathetic nervous system is activated, and the brain prepares the body to fight or flee. A cascade of hormones drives a physiological response, releasing epinephrine and norepinephrine to elevate heart rate and breathing rate and increase arousal, a combination of sensations that can feel scary and overwhelming for parents uniquely triggered by different situations and concerns. Then, the hypothalamic-pituitary-adrenal (HPA) axis is activated, releasing a second set of hormones that dump cortisol into the bloodstream to keep parents alert. When a threat persists, such as a prolonged hospital stay, chronic exposure to these hormones can drive the body into a grueling state of hypervigilance.
“Kangaroo care can help release oxytocin. So that’s associated with feelings of relaxation and bonding, which really can help reduce stress and anxiety levels in parents,” said Pamela A. Geller, Ph.D., a Drexel University professor and psychologist specializing in perinatal mental health and the NICU experience. Oxytocin tamps down the HPA axis, mitigates the stress response, and calms the nervous system. Geller emphasized the value skin-to-skin care offers all parents, including fathers and other nonbirthing parents, but especially to parents of NICU babies who don’t have the same opportunity to interact in ways that stimulate oxytocin to help offset the additional stress that comes with having a baby in the NICU.
“Oxytocin helps promote and improve parental mood and feelings of attachment and competence. Parents feel more confident in caring for their infants and more in tune with their baby’s needs,” Geller said. “It also helps parents learn how to manage their emotions better and improve coping skills as a potential way to moderate their anxiety. It reduces the risk of postpartum depression.”
While more research is needed to appreciate the extent to which SSC protects against mental illness for fathers and nonbirthing parents — who may show different symptoms of stress and coping strategies — SSC’s social and psychological benefits extend beyond the person who has given birth, Geller said. Armstrong echoed, “Partners can feel more out of control at times than the mom. They want to help you and they want to help the baby, they just don't know what to do.”
Not all babies who need NICU services are born preterm or have low birth weight. SSC offers an easy way for all parents to connect with their babies and feel a sense of purpose knowing there is something only they can provide for them. “Kangaroo care makes you feel like a parent,” Armstrong said, “and that your baby, even if sick or unstable, isn’t as fragile as they look. Over time, parents are happier, calmer, and more confident.”
***
Like many NICU parents, it took me years after each birth to feel like myself. Writing to process and share my experience helped me feel less alone. Time also showed me my children: healthy, sturdy, and strong. I slowly checked off the apnea monitors, retinopathy of prematurity, heart defects, and speech delays — the ongoing medical concerns that followed us long after the NICU. In perinatal and postpartum mental health support groups — I later became a peer facilitator for Postpartum Support Virginia — we teach that PMADS can be treated with some combination of social support, self-care, talk therapy, and medication, a path-to-healing “cocktail” unique to each person. For me, nursing my preemies into toddlerhood was a source of pride and enduring connection I cherished. Moving my body and spending time in nature helped me close the cortisol loop. Around the two-year mark, there was a turning point when I would begin to sleep through the night because my toddler was too. Accessing therapy in the NICU the second time around and continuing into Winslet’s third year helped me process and make sense of my experience, and eventually, medication helped me realize I didn’t have to live with anxiety and post-traumatic stress.
Today, Winslet is a thriving 8-year-old with a wild imagination and a flair for dance, but when she was born, I didn’t know what the future held. The only thing I knew for certain was we were safe when we were together. In those moments, when I could see and feel her and respond to her cues with my voice and touch, I came to know Winslet as my girl and myself as her mama. Holding her was pain relief. Being with her was like plugging in to re-regulate my brain and recharge my body and heart to find the courage to keep going.
Jacqueline Sears
Jacqueline Sears, MPH, CPH, CBS, is a two-time NICU parent with a degree in biomedical engineering and a master’s in public health epidemiology. Jacqueline’s most recent work lives at the intersection of mothering redefined, public health, and empowered parenting in preterm birth, the NICU, and beyond. She is a graduate student in the Johns Hopkins University M.A. in Science Writing program. Jacqueline writes on maternal and child health topics, focused on equity in access to parenting interventions that promote attachment and human milk feeding in the NICU.
Senior Editor: Lindsey Leake
Art Editor: Veronica Tremblay
Copy Editor: Christopher Graber