An Infectious Cure: Oncolytic Viruses and Glioblastoma
Viruses are opening oncologists’ eyes to new treatment possibilities for the world’s most intractable brain cancer
by Avigial Albert
December 15, 2024
Like unwelcome houseguests, brain tumors come in a variety of unappealing archetypes. There are meningiomas, which take up space in a membrane called the meninges. Oligodendrogliomas squat in and eventually destroy nerve linings. And the poetic-sounding but brutally prosaic astrocytomas hitch themselves, with varying levels of aggression, to astrocytes, the star-shaped cells that compose the skeleton of the neuronal support network.
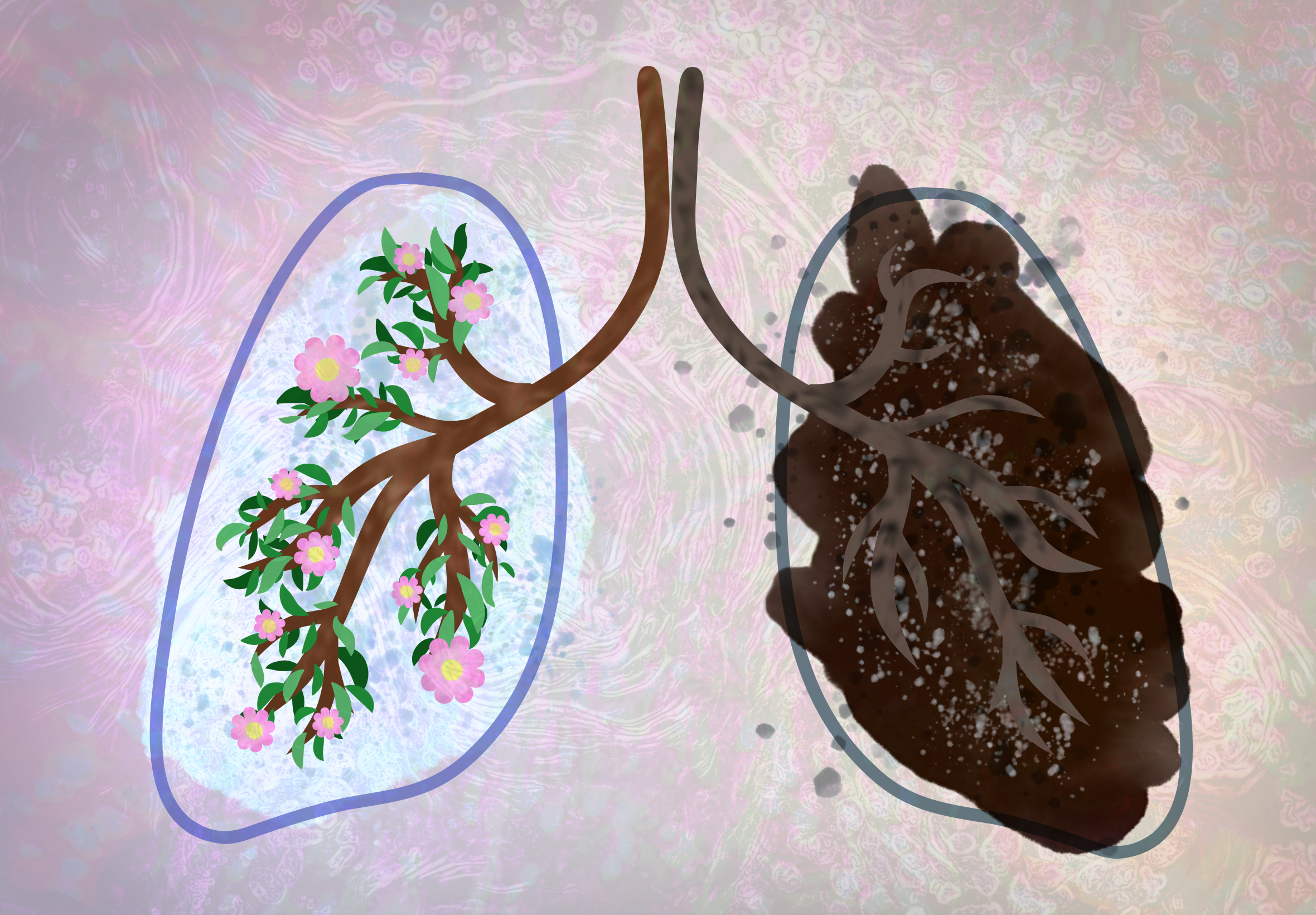
If you think of a regular astrocytoma as a distant star blinking out, then its most severe presentation, glioblastoma, is a supernova. A particularly efficient tumor that, according to the American Association of Neurological Surgeons, kills about 60% of patients within a year, glioblastoma is notoriously hard to treat for two reasons. First, it tends to grow “fingers” that take parts of the brain hostage and prevent complete surgical removal. Second, the blood-brain barrier makes glioblastoma tumors inaccessible to most chemotherapy drugs.
Researchers estimate that 300,000 people are diagnosed with glioblastoma each year globally. This accounts for more than half of patients diagnosed with primary malignant brain tumors, 93% of whom will be dead within five years, according to the National Brain Tumor Society.
Although glioblastoma was first identified in 1863, we still have no cure for it. In 1999, the Food and Drug Administration (FDA) approved the chemotherapeutic drug temozolomide, which, in conjunction with radiation and surgical removal of the primary tumor, became the standard of care for glioblastoma. But people still died in droves, and in 2000, the National Academy of Sciences deemed glioblastoma “the terminator.”
It’s hard to think of something to do besides watch said terminator do its grisly work. But in a biological twist, getting sicker — the right kind of sick — may be the answer. Catching a virus such as herpes simplex, polio, Zika, or measles may not sound like a good idea for a patient already struggling with terminal disease, but for oncologists these infections represent a promising frontier for cancer treatment: oncolytic virotherapy. Recent research has shown that, with some intervention from scientists, these particular biological assassins can edit their hit lists to only target cancer cells. Scientists call viruses that target cancer cells “oncolytic,” from the Greek root onkos, meaning mass or tumor.
Viruses, which are composed of genetic material — either DNA or its thinner sister, RNA — need host cells to reproduce. So, when they enter an organism, their first order of business is to locate some cells in which to replicate. In the case of many viruses, if replication continues unchecked, viral material will soon strain host cells to the breaking point, causing lysis (cell death) by rupturing.
Scientists have long studied the curious link between infection and cancer regression, in some cases. And the concept of viruses as a cancer treatment isn’t new. In 1904, George Dock, M.D., an internist and professor of medicine at the University of Michigan, documented the case of a leukemia patient who entered temporary remission after contracting the flu. “A ... satisfactory explanation of the changes observed in [this case] under the influence of [influenza] does not seem possible at present,” he wrote. “We are still too much in the dark.”
Dock was onto something, though, and other scientists started noticing the pattern. In 1953, Howard Bierman, M.D., of the National Cancer Institute at the National Institutes of Health, watched a leukemia patient catch chickenpox, caused by the varicella-zoster virus, and subsequently enter temporary remission.
While these cases were incidental, scientists began considering deliberately infecting patients. The 20th century saw experiments in which cancer patients were infected with viruses, such as hepatitis, West Nile, and mumps. Between the 1940s and 1970s, researchers in countries including the United States and Japan tested common viruses on a range of cancer types and reported success rates ranging from 15 to 90 percent. One thing was certain: viruses did something.
In 1991, a research team led by Robert Martusa, M.D., of Harvard Medical School, published the first study on genetically engineered, cancer-killing viruses. He administered a weakened form of the herpes simplex virus to mice with brain tumors and although most died, his study marked a watershed moment in cancer research. By controlling viruses more precisely — manipulating their genes to only seek out cancerous cells, for example — scientists hoped to maximize efficacy while minimizing collateral damage.
Since then, millions of dollars have been invested into the study of oncolytic viruses and dozens of clinical trials undertaken. In 2015, the FDA approved talimogene laherparepvec (called IMLYGIC) for the treatment of melanoma. But most oncolytic virotherapies, including those indicated for over a dozen cancers (glioblastoma among them), are still in the trial phase. Because such clinical trials might be a glioblastoma patient’s best shot, they don’t lack for participants.
Long before patients enter the picture, though, researchers must determine which virus to use. Maciej Lesniak, M.D., head of Northwestern University’s neurological surgery department, chose adenoviruses, the cause of the common cold, for his 2017 clinical trial. These viruses are extremely infectious and relatively low risk, making them ideal candidates for oncolytic viruses, which must infiltrate the cancer patient’s immune system to work but are not intended to introduce a new illness. Scientists can also edit the adenoviral genome fairly easily, narrowing the viruses’ target range to cancer cells and further reducing risk of pathological infection. According to study coauthor Christina Amidei, M.D., Northwestern’s Director of Clinical Research, Neurological Surgery, Lesniak did exactly that — and patented the result — before conducting his trial.
For the average trial patient, an oncolytic virus’ journey starts in a syringe. From there, researchers have two options, explained Christopher Alvarez-Breckenridge, M.D., Ph.D., a neurosurgeon at the University of Texas MD Anderson Cancer Center in Houston. The virus can be administered straight into the tumor, but since direct brain injections have a high risk of harmful infection, doctors may instead choose to introduce the virus by inserting a stem cell during resection.
Amidei’s team took that route, injecting virally loaded neural stem cells into patients’ brains immediately after surgically removing the primary tumor. “You can think of it as the engine of a train,” said Amidei of the stem cells. “The oncolytic viruses are all the cars that follow the engine.” Because stem cells can travel farther than viruses, tethering the viruses to the cells enables the viruses to diffuse more deeply into the area, thus accomplishing a more thorough cleanup.
Once it reaches the tumor site, the virus will infiltrate cancerous cells and replicate there. Then, “it takes over the machinery,” Alvarez-Breckenridge said. Just as the cancer imposed itself on the body, the virus now does the same in the cancer cells. In each cell it enters, the virus reproduces rapidly, filling the cell until it bursts and, as a bonus, freeing its genetically identical descendants, which fan out to find more cancer cells.
In addition to destroying cancer cells, a virus also acts as a beacon for the body’s immune system. Depending on the case, a “tumor microenvironment can change in terms of being more proinflammatory or more immunosuppressive,” Alvarez-Breckenridge said. “Tumors generally like to have it more immunosuppressive because inflammatory processes can be detrimental to the tumor.” Viruses, as foreign bodies, are effective initiators of these inflammatory responses.
That last point, he said, is important when it comes to brain cancers, since the central nervous system is generally immunosuppressive even when healthy, and “gliomas tend to co-opt that system.” In other words, the body may not even be aware of the presence of a brain tumor until a virus enters the equation and puts that area back on the immune system’s radar. The virus itself attacks the tumor, and the immune system deploys white blood cells to destroy the virus, which includes destroying its host cells. These combined efforts create a two-fronted assault on the tumor. So if oncolytic viruses can do what they are designed to do, glioblastoma’s terminator status could become a thing of the past.
As of February 2023, 21 oncolytic viruses targeting glioblastoma were in trials, but none had been approved for market by the FDA. “They haven’t gotten to the point where they’re being compared to the standard of care,” Alvarez-Breckenridge said. “The studies that have been done up to this point are limited in their ability to, in a robust, statistically sound fashion, say: ‘This oncolytic virus is better than the current standard of therapy.’”
Conceptual visualization of the herpes simplex virus surrounded by antibodies. Image credit: iLexx via Storyblocks
The holdup? “They’re expensive,” Alvarez-Breckenridge said. “They require a lot of buy-in.” Amidei agreed, describing Lesniak’s adenovirus as “expensive and difficult to manufacture” because of its biological, as opposed to synthetic, nature. Oncolytic viruses fall into a category of drugs known as biologics, products found in living organisms. Biologics are more sensitive to microbial contamination than synthesized drugs, necessitating costly antiseptic precautions during their production.
There’s also the fact that oncolytic viruses don’t function in a vacuum, which leads to questions like: Why do some patients have better outcomes than others? “Did those patients respond better because there’s something unique about the biology of the tumor or their immune system or something else that’s driving them to do better?” Alvarez-Breckenridge said. “Or, is the virus actually taking advantage of something within those patients that causes them to do better? We don’t know.”
Still, scientists remain optimistic. Lesniak’s team recently completed its five-year follow-up with the remaining trial patients and has endeavored to lengthen the stem cells’ and viruses’ lifespans and, by extension, they hope, the lifespans of their patients. Amidei gave an emphatic, “Yes, yes” when asked if oncolytic viruses would eventually become a viable treatment for glioblastoma. Aside from oncolytic viruses’ potential, corresponding research has also broadened understanding of cancer treatment. In contrast to treatments like temozolomide, oncolytic viruses “explore the tumor microenvironment,” Alvarez-Breckenridge said, shining a spotlight not on the tumor, on which treatments typically focus, but on the ground from which it grew.
Avigial Albert
Avigial Albert is a technical and creative writer based in Baltimore. A graduate of the Johns Hopkins Master’s in Science Writing program, she taught high school English for several years before moving into her current role as a federal technical writer. She is also a freelance writer/editor who has published creative nonfiction pieces on topics including grief and young adulthood. Having lived through loss at a young age, she is a strong believer in supporting bereaved families and raising awareness about treatments for terminal illnesses.
Senior Editors: Lindsey Leake & Kristen Hines
Art Editor: Rachel Lense
Copy Editor: Christopher Graber