Near Certain Failure
For life-threatening hydrocephalus, the standard solution is one that fails
Image credit: Pete Linforth via Pixabay, edits by Rachel Lense for The Science Writer
by Trish Carrington-Adkins
February 21, 2024
When I initially heard my daughter, Lily, gag from her third-floor bedroom, I worried she was sick. She said it was just a reaction to something gross she smelled. I believed her. It was easier that way.
Other abnormalities followed over the next two weeks. She stumbled in the space between the car and the curb at high school drop-off. I told myself that anyone could have stumbled in that space; the curb was rather high. At her dance recital, Lily seemed supernaturally dizzy, an out of control spinning top threatening to tumble off the stage. The next week, she fell asleep in the car after rowing practice, exhausted, it seemed from pulling herself across the water.
Then Lily vomited in front of us, twice, in our kitchen sink.
We knew and she knew: we needed to get to the emergency room. It wasn’t the first time this had happened and most likely, it won’t be the last.
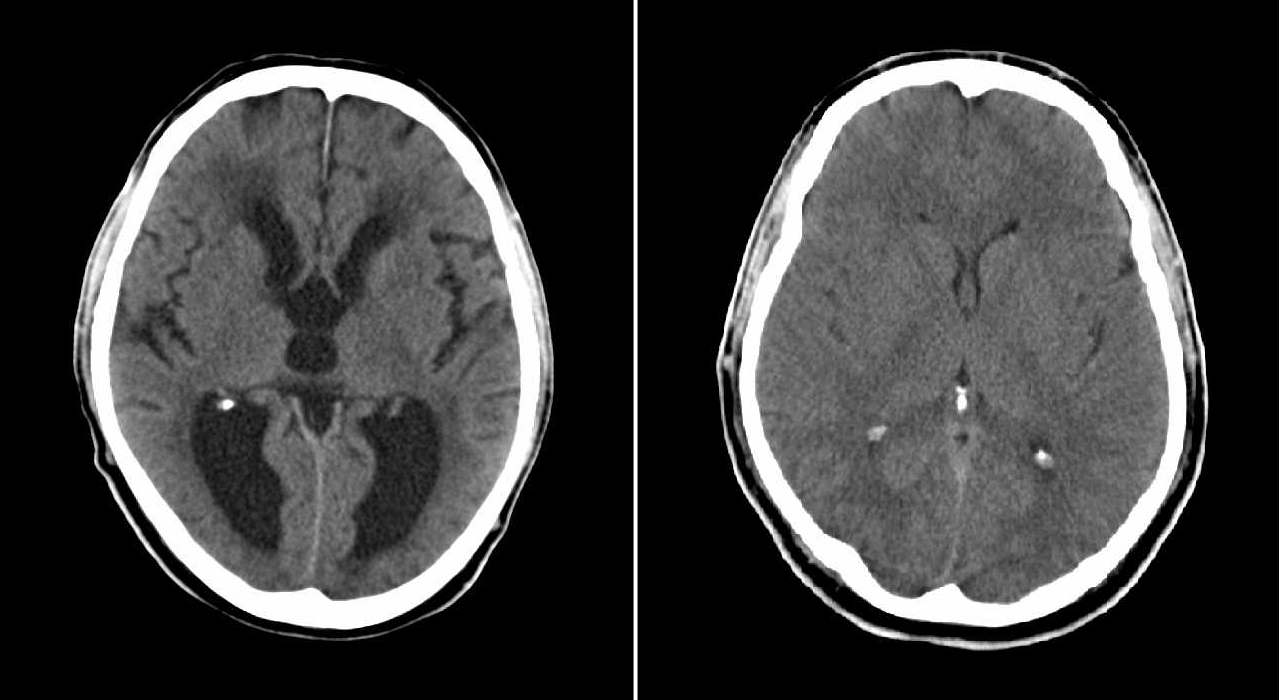
A side-by-side comparison of a brain with hydrocephalus (left) and a brain without hydrocephalus (right) as documented through computed tomography scans. Image credit: MBq via Wikimedia Commons (public domain), edits by Rachel Lense for The Science Writer
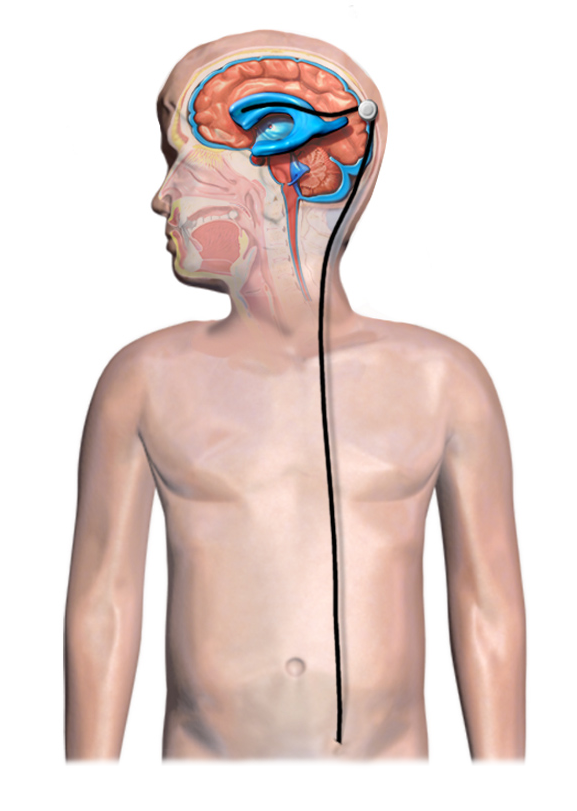
Lily has hydrocephalus, a condition caused by an excess of cerebrospinal fluid (CSF) — a clear, champagne-colored liquid that surrounds our brains and spinal cords. When she was a baby, a brain tumor blocked the natural flow of CSF, flooding her brain and filling the already crammed quarters of her cranium, raising the pressure to unmanageable levels. Surgery and radiation removed the tumor, but the hydrocephalus remained. The solution: a ventriculoperitoneal shunt placed in her head to drain the excess CSF that her brain cannot absorb into her abdomen.
Hydrocephalus comes in various forms — it can be congenital or acquired via injury or illness. Common disorders of the circulation of CSF include normal pressure hydrocephalus, which most often affects older people, and idiopathic intracranial hypertension, which almost exclusively affects women of childbearing age. Although the symptoms associated with these conditions may be serious, not everyone needs a shunt. But when hydrocephalus produces life-threatening pressure in the brain, a shunt becomes the standard option. With it, people can live regular lives. Lily goes to school. She rows competitively. She dances. She travels. But she does it all while knowing the address of the nearest emergency room with a neurosurgery team because ventriculoperitoneal shunts are notoriously unreliable. Studies estimate that 40% of VP shunts fail within two years of implantation and 98% fail within 10 years. Lily’s has already failed twice, and there is no way to know — no shunt crystal ball, no CSF fortune telling, no hydrocephalus seer who can predict where she’ll be — when it fails again.
Lily’s shunt saves her life every day. But when it fails, her life is immediately at risk.
***
Hydrocephalus is sometimes referred to as “water on the brain”; however, CSF is actually a nutrient-rich fluid that cushions and bathes the brain and spinal cord in calcium, magnesium, and sodium, ensuring that the central nervous circuitry works. The choroid plexus, a complex system of capillaries lined with specialized cells, continuously secrete CSF — approximately 5 fluid ounces, or a glass of wine, a day. Inside the brain, four interconnected ventricles work to circulate the fluid, absorbing and replenishing it around the clock.
As a baby, a tumor invaded Lily’s brain and grew aggressively, staking its claim in an already crowded environment. The tumor blocked the flow of CSF, and her ventricles could not keep up with the non-stop production. When we looked at her CT scans, doctors would point out her swollen ventricles, which looked like lakes of dark water. It reminded me of an aerial view of hurricane-flooded landscapes, structures unrecognizable underneath the flood.
Outside of the brain, hydrocephalus manifests in all sorts of ways. People have reported sudden bouts of blindness, extreme pulsating headaches, and mental confusion. It can also appear in more innocent ways, like as an upset stomach. Hydrocephalus can look like a nap in the car after a hard workout or a stumble on a tall curb, but it can also become a living room full of emergency medical personnel, police officers, and terrified parents begging for the quickest ride to the children’s hospital.
***
While there are different types of shunts, all work with the same three parts: the ventricular catheter in the brain, which Lily has always called her “bumps,” and a valve that connects it to a long piece of spaghetti-like tubing that extends down along the right side of her neck and into her abdominal cavity, where the excess CSF is drained and absorbed. On her stomach, Lily has two scars — tally marks from the original shunt insertions. On her head, she has four: two to match her belly and two more for the two shunt revisions.
A diagram of typical shunt installation in a child with hydrocephalus. Image credit: Blausen Medical Communications via Wikimedia Commons (CC BY-SA 4.0), edits by Rachel Lense for The Science Writer
It is the ventricular catheter that most often fails, especially in pediatric patients, according to Carolyn Harris, Ph.D., associate professor of chemical engineering and materials science at Wayne State University in Detroit; however, the mechanisms that lead to failure are not totally understood.
Since their early days, shunts have been made of silicone, a material that is safe for the body, but one with a relatively “sticky” outside surface. Shunts removed (or explanted) from patients are covered in an array of cellular materials, including astrocytes — cells that perform immune system functions in the brain. Astrocytes seem to flock to shunts, sticking to them and recruiting more astrocytes to the cause of ousting a foreign body. In her lab, Harris and her team conduct experiments on failed shunts to study what types of cells are obstructing and clogging these devices and determine the environmental and biological factors that might contribute to failure.
No one can predict when a shunt will fail. There aren’t always warning shots, like my daughter’s stumbles and fatigue during her second shunt failure. Her first failure was swift and dramatic. Lily was fine one moment and the next, vomiting uncontrollably and close to losing consciousness. That time, Lily’s neurosurgeon described her removed shunt valve as completely blocked, almost walled off. The signs of damage were more subtle on the second shunt Lily had removed: tiny holes along the shunt valve were filled with cellular barnacles.
“Biology is opportunistic, and it will continue to try and block the catheter until it thinks it’s done,” Harris said. Having studied shunts almost her entire research career, she wonders at solutions, such as convincing the astrocytes that the shunt isn’t an invader or that they’d already evicted the unwanted guest.
For people with shunts, solutions cannot come fast enough. In 2022, the Hydrocephalus Association published the results of a survey of 890 hydrocephalus patients and caregivers. The respondents’ top research requests centered on the need for less invasive procedures, improved access to care, and a one-time therapy that didn’t fail.
When I ask Lily if she fears shunt surgery, she just shrugs. The surgery, she says, is “like magic.” And it is. Once the clogged, debris-ridden shunt is removed, the new catheter manages the flooding inside Lily’s brain, and the symptoms of hydrocephalus disappear. But, when I ask her about her feelings on the probability that the device will fail, the answer is a resounding “I hate it.”
In Detroit, Harris’s team and clinical collaborators have collected around 550 explanted shunts, examining the sticky, obstructive cells under a microscope and then correlating those findings to information about the shunt’s previous owner. How long did they have the shunt? How old were they when it was implanted? How many revisions had they had in the past? Her team also uses a “brain on a bench” model, recreating the intracranial conditions in a plastic enclosure and using a pump system to simulate CSF flow and pulsation rates within the central nervous system. Since the brain is such a small space, Harris says, even a patient’s cough might influence the failure of a shunt, moving it closer to the ventricle wall and causing it to suck in cells that could clog it.
That work has translated into several experimental coatings, including one derived from an over-the-counter antioxidant supplement called acetylcysteine, which breaks down mucus in the body. When this coating is painted onto a shunt, it makes it less sticky. With fewer spots to attach to, cells simply move along, leaving the shunt alone.
There is still more research to be done, but Harris believes the field of study is evolving quickly — not just in her lab but in labs everywhere.
We have about nine months until Lily goes away to college. She is evolving quickly from my daughter the child to my daughter the young adult. We talk endlessly about her shunt, and she’s picked potential colleges based on their proximity to a hospital with top neurosurgeons. It’s stressful for any parent to push their child out into the world, but my husband and I have the added pressure of knowing that our daughter’s shunt could pull her back to the emergency room at any time. We know it isn’t likely the science evolves quickly enough for Lily’s freshman year. We know her shunt could fail again, and that again could be tomorrow, or the next year, or if she’s lucky, never. It’s luck we wish for now, and it is science that we have hope in for the future.
Trish Carrington-Adkins
Trish Carrington-Adkins is a science writer, childhood cancer research advocate, and lover (of birds). You can find her writing about her adventures on her blog Yoke, sharing childhood cancer research stories on The Childhood Cancer blog, and working on essays about how science moves in her own life. Trish has a journalism degree from Temple University and is a candidate in the Johns Hopkins University Science Writing graduate program.
Senior Editor: William Kucinski
Art Editor: Rachel Lense
Copy Editor: Kristen Hines